Women in lesbian relationships share many of the same health risks with women in general, although discrimination and prejudice can increase barriers to receiving proper and comprehensive healthcare. If you identify as lesbian or bi-sexual, you’ve probably experienced this.
Whether they realize it or not, when treating you, healthcare providers may act in ways that are explicitly or implicitly homophobic. They may not be educated in healthcare issues that affect queer populations, or they don’t ask the right questions. You may have a hard time “coming out” to your provider, or skip going to the doctor altogether to save yourself the time, trouble, and embarrassment.
If your healthcare provider can’t be relied upon to bring up the issues that may affect you, you have to take your health into your own hands and make sure that you ask your doctor the important questions. The Gay and Lesbian Medical Association (GLMA) website has published a list of ten topics that you should discuss with your healthcare provider.
- Breast cancer: there may be more risk factors that apply to lesbian patients, and less screening exams done. Risk factors include pregnancy after the age of 30, no pregnancy, a positive family history of breast cancer, and being part of a population that may see doctors less often. The current recommendations for breast cancer screenings have changed in the past few years. Mammograms should be done at the discretion of the patient after the age of 40, and should be done yearly after the age of 45.
- Depression/anxiety: chronic stress from discrimination is worse when lesbians are afraid to “come out” to their providers. The overall rate of anxiety and depression in our country is high. Little is known about the actual occurrence rate but dealing with family and a society that lacks understanding about who you love makes it worse. In the winter, seasonal depression can add to this as well. If you suffer from Seasonal Affective Disorder, a luminotherapy lamp and Vitamin D3 can help.
- Heart disease risk: Some risk factors for heart disease that affect the lesbian population are obesity and smoking. Yearly medical exams to check blood pressure, lipids and diabetes are recommended. Ask your family for your family history of diseases and discuss them with your doctor. Get your cholesterol checked every few years.
- Gynecological cancer: Lesbians are more at risk for some kinds of gynecological cancers. More instances of HPV (which can, in some cases, lead to cervical and vulvar cancer), ovarian cancer and endometrial cancer have been documented in lesbians. Additionally, obesity increases risk for hormonal cancers including uterine and ovarian cancer. Regular pap tests and pelvic exams are essential.
- Fitness: Studies show that obesity is more common in lesbians, as is sedentary lifestyle. This increases the risk for heart disease, cancer, and diabetes; but also degenerative joint disease. Exercise is good for everyone. Healthcare providers can give advice about adopting healthy lifestyle habits, including diet and exercise.
- Tobacco: Lesbians smoke more often, even if only socially. Smoking is associated with higher risk for cancer, heart disease and COPD. Quitting smoking is a difficult process, but one that your healthcare provider can help you through.
- Alcohol: Heavy drinking and binge drinking are more common among lesbians. This can lead to cancer, liver disease and obesity.
- Substance use: Lesbians use drugs more often, sometimes due to stress from homophobia, sexism and/or discrimination. An adoption of healthier habits to deal with stress can be a topic to bring up with your doctor.
- Intimate partner violence: Lesbians need to be asked about violence and have access to welcoming counseling and shelters when needed. Domestic violence is unfortunately common, and so are unhealthy relationships with co-dependency. Psychological health affects physical health. If you’re worried about the crossover between these two issues, discuss your relationship with your doctor, and ask for referrals when necessary.
- Sexual health: Lesbians can get the same sexually transmitted infections as heterosexual women. Skin-to-skin contact, mucus membrane contact, vaginal fluids and menstrual blood can transmit STDs. Sexually transmitted infections such as human papillomavirus (HPV), trichomoniasis and bacterial vaginosis (which is not an STD, but an infection that can make it easier to transmit an STD) can spread between women. Oral sex, digital-vaginal, and digital-anal contact, especially with shared penetrative sex toys, can spread infections. HIV can be transmitted as well. Ask your healthcare provider about screenings, as well as protection methods.
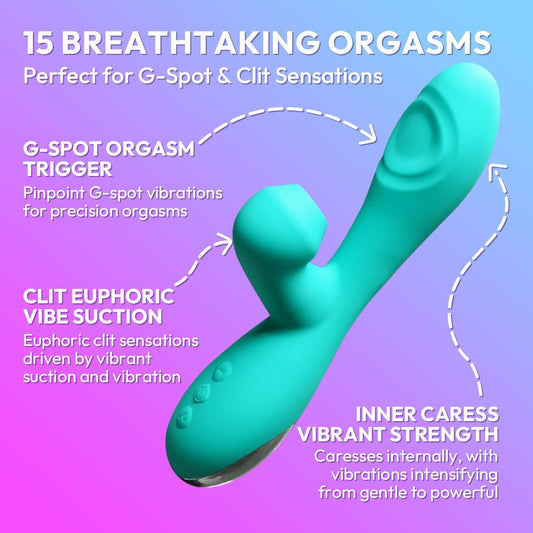
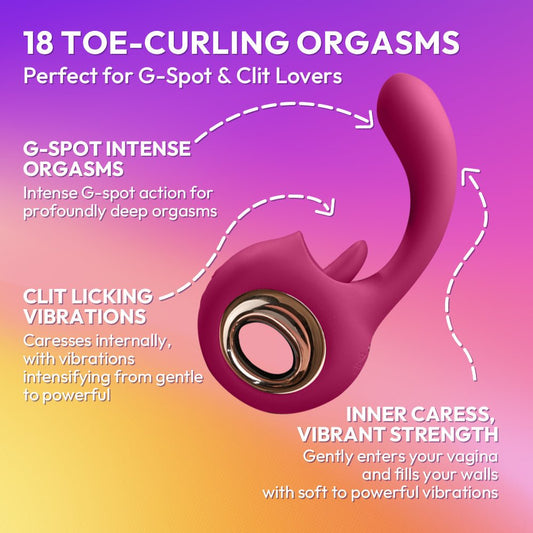
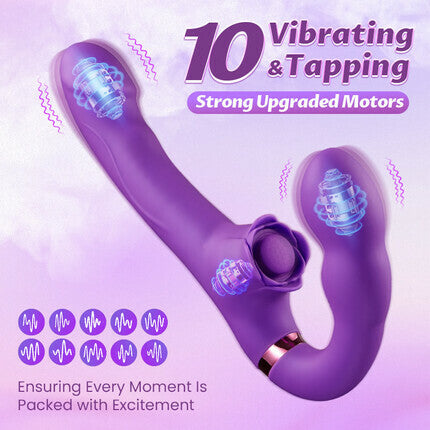
As for actions you can take in your everyday life to protect yourself, start with safe sex. To protect yourself from sexually transmitted infections, get tested and have your partner tested. Have a frank conversation with your partner about sexual health. Wash your hands before and after sexual activity. People may not know that they are infected and others might not be honest about their health. If you use recreational drugs, don’t share needles, and get vaccinated for hepatitis A, hepatitis B, and HPV if possible. Use barrier protection (such as a condom, latex sheet, dental dam, or glove) to avoid contact with menstrual blood and genital sores. Do this every time you have sex. If you use sex toys, cover them with a new condom each time the toy is used for a different person. Use gloves and lubricant for sexual activity that may cause bleeding. Do not go from the rectum back into vagina, or use a new condom as it spreads bacteria and causes vaginal infections.
The GLMA, WPATH and your local Pride Center or Planned Parenthood usually have a list of LGBTQAI+ friendly providers.
These providers generally are aware of your barriers to care and should be safe to come out to and discuss your health care issues with. They should also be aware of your preventive health care needs and offer you screening and vaccinations. This health care provider can also refer you to understanding therapists or specialists. Plus, you can talk about anxiety, depression, your relationship, your substance use, your preventative care, and any other health concern you may have.